Fraud, waste and abuse (FWA) ravages the US health care system. Estimates from the National Health Care Anti-Fraud Association show fraud costs health care organizations $70 billion to $230 billion each year. The precise figure is unknowable because only 3 to 10% of this fraud is ever detected.
With more data in health care than ever before, what is the opportunity to use artificial intelligence (AI) and other advanced analytics techniques to improve fraud detection?
That was the topic of a recent webinar featuring Prime Therapeutics, the pharmacy benefit manager that Fast Company named among the world’s most innovative companies for 2020 for their use of SAS® Detection and Investigation for Health Care to fight fraud, waste and abuse. SAS Medical Director Steve Kearney, PharmD, hosted the webinar.
How it works
Prime Therapeutics integrates pharmacy and medical claims into an advanced analytic engine to identify cases for their investigators. Then they utilize machine learning models and other artificial intelligence (AI) techniques to sniff out the multiple fraud schemes deployed by pharmacies, prescribers and members.
With these new capabilities, Prime Therapeutics saved its clients $355 million in 18 months. As Anne Mack, Senior Director for Pharmacy Audit and FWA at Prime Therapeutics explained, “This could not have been discovered with pharmacy data alone.”
During the webinar, Anne Mack described how analytics helps break multiple types of fraud schemes, including those from pharmacies, prescribers, and members. Some of the schemes include phantom pharmacies, reselling samples or products from wholesale, creating compounds with non-FDA approved ingredients, member number fraud and false telemedicine claims, including ones for durable medical equipment and pain creams. Constant evolution of fraud schemes, as well as increased sophistication and use of technology by the fraudsters, means that pharmacy benefit managers need to actively monitor emerging fraud rings in order to protect clients.
Detecting new fraud schemes
Given our current public health crisis related to COVID-19, Dr. Kearney discussed how FWA will continue to evolve in new ways. Anne Mack presented a case study from a pharmacy during the pandemic involving a prescription multivitamin. With the help of advanced analytics, investigators at Prime detected that a pharmacy was claims phishing. The investigation identified a pharmacy that was fraudulently promoting the multivitamin as COVID-19 treatment, lacked prescription orders and waived copayments. Based on the investigation, the pharmacy was terminated from the network and reported to the board of pharmacy, as well as law enforcement.
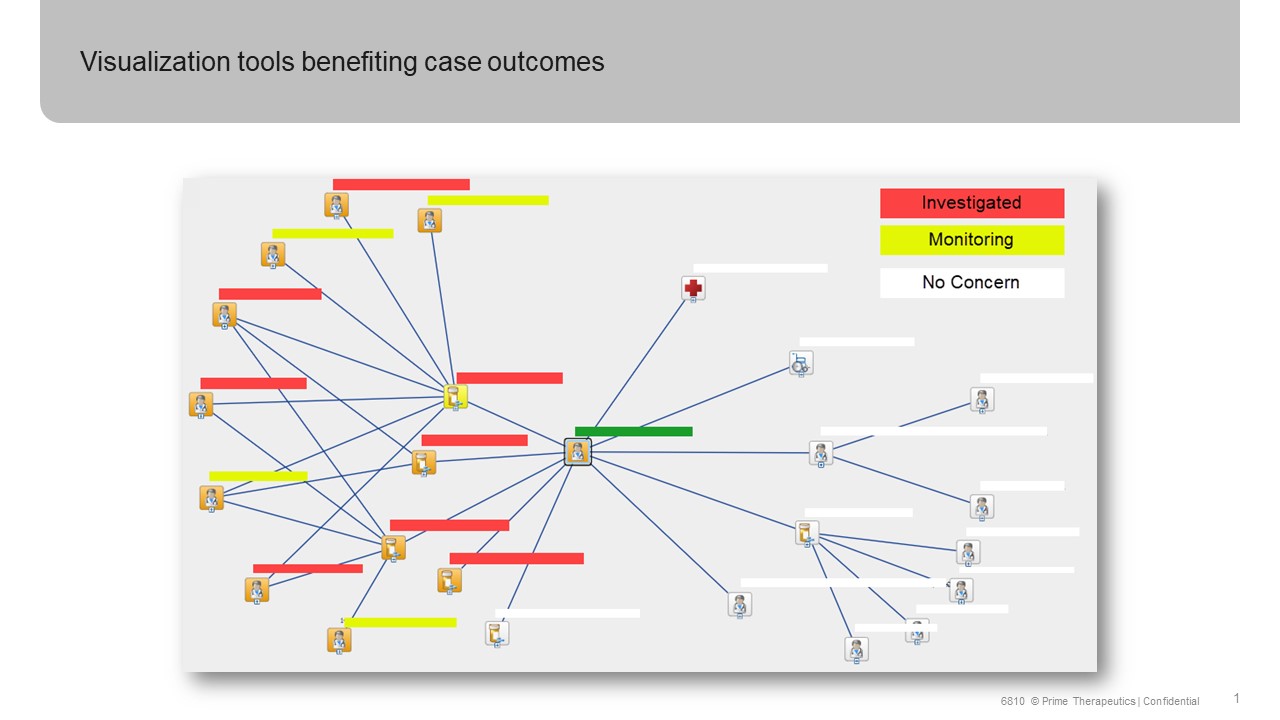
Effective fraud detection goes beyond algorithms alone. Visualization of social network analysis enables investigators to make much quicker connections between parties involved in fraud schemes (see Figure 1 below).
Tackling fraud, waste and abuse requires collaboration across pharmacy benefit managers, such as Prime Therapeutics, as well as government health officials and care providers. The important work of identifying pill mills through prescriber data and doctor shopping through member claims data has led to some progress in the war against the opioid epidemic. The American Medical Association’s Opioid Task Force 2020 Progress Report shows a 37% decrease in opioid prescriptions between 2014 and 2019. “Despite these efforts, illicitly manufactured fentanyl, fentanyl analogues and stimulants (e.g. methamphetamine, cocaine) are now killing more Americans than ever”, according to this year’s report.
This is a heartbreaking statistic and one that calls us to action across the health ecosystem. Together, supported by waves of new data and technology including AI, organizations can work together to reduce the fraud waste and abuse present in the health care system globally.
If you want to learn more about specific steps your organization can take using AI to curb FWA, please watch the free on-demand webinar Catch a Fraudster: Finding the needle in the haystack with AI.
SAS is a long-time member and partner of the National Health Care Anti-Fraud Association (NHCAA), the leading national organization focused on the fight against health care fraud. Their members comprise nearly 90 private health insurers and those public-sector law enforcement and regulatory agencies having jurisdiction over health care fraud committed against both private payers and public programs. This webinar was organized jointly between SAS and NHCAA.
