In spite of years of research and recommendations on bone health, we still have considerably high rates of osteopenia and osteoporosis in the US. That leads us to believe we haven’t yet uncovered all we need to know about protecting our bones. But, thanks to new research we’re learning new strategies for slowing bone loss.
Bone Remodeling
Our bones are continuously being remodeled by way of bone cells called osteoblasts (cells that form new bone) and osteoclasts (cells that break down bone). The rates of bone building and bone breakdown change throughout our lifespan. Our peak bone building years are between birth and age 25 when the bone building osteoblasts lay down more bone than the osteoclasts break down. Between 25 years and 50 years (unless a woman has early menopause), we add and break down bone at an equal rate. After 50, due to hormonal changes of aging and other considerations, women and men begin to break down bone faster than we add it. This is when our risk for osteoporosis is greatly increased so this is especially a time when we need to step up our nutrition and lifestyle strategies for maintaining our bone mass.
Common strategies for building strong bones have come under scrutiny over the past few years leaving folks perplexed about the best practices for bone health. This blog will provide a summary of the latest recommendations for bone health including a few new kids on the block.
Nutrients for Bone Health
Calcium
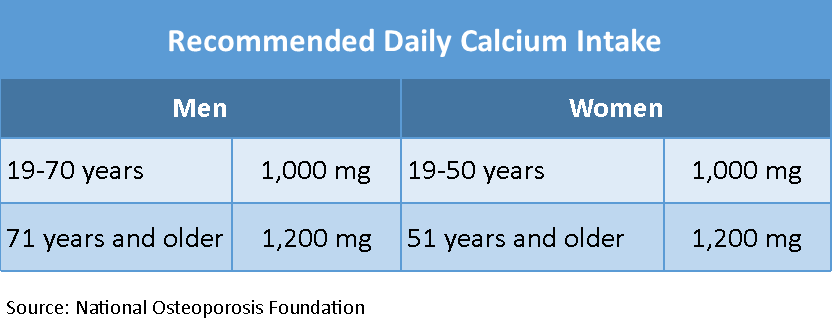
The National Osteoporosis Foundation in the US recommends the following calcium intake daily.
Calcium recommendations vary worldwide, however. According to bone health expert, Carolyn Dean, MD, ND, the UK recommends a daily allowance of 700 mg for women and men 19+ years and the WHO recommends 500 mg per day.(1) A Swedish study suggested that 700 – 800 mg/day of calcium per day appeared to be the tipping point beyond which further calcium supplementation did not offer additional bone health benefits.(2,3) In addition, nutrition researcher, Walter Willett, MD, Dr.P.H., chair of the Department of Nutrition at Harvard’s School of Public Health, also suggests that the U.S. calcium recommendation may be higher than needed and Vitamin D is lower than needed. Dr. Willett feels the WHO recommendation of 500 mg per day may be adequate and the UK’s recommendation of 700 mg leaves a little safety leeway.(4)
Researchers do agree that when possible, getting your calcium from natural dietary sources is the best advice because a meta-analysis of calcium supplementation studies suggested that taking more than 500 mg per day of supplemental calcium can cause an increased risk of heart attack in some people.(4)
Check out this list of dietary calcium sources and non-dairy calcium sources.
For those unable to meet their daily calcium goal with diet, a calcium supplement of up to 500 mg per day of supplemental calcium in a highly absorbable form (i.e. citrate or hydroxyapatite) is ok if your supplement also contains adequate amounts of other important bone nutrients – Vitamin D3, magnesium, boron, zinc, copper and Vitamin K2.
Note: When assessing your daily calcium intake from supplements, remember to include the calcium from the calcium-fortified foods like: calcium fortified juices, cold and hot cereals and tofu. These foods have been supplemented with calcium so they should be included in the 500 mg daily calcium supplement maximum.
Vitamin D
A major role of Vitamin D is to keep blood levels of calcium and phosphorus in the normal range. It also helps your body effectively absorb calcium. Very few foods naturally contain Vitamin D. The major sources of dietary vitamin D are egg yolk, Vitamin D fortified milk, and fatty fish and their oils (example – cod liver oil). For more sources of vitamin D, check out THIS LIST.
Ninety percent of our Vitamin D comes from sunlight exposure which converts cholesterol in our skin to Vitamin D3. Aging, sunscreens and other factors can interfere with this natural conversion which puts many people at risk for Vitamin D deficiency. It is a good idea to know your blood level of Vitamin D to assess whether your current diet and lifestyle are maintaining healthy blood Vitamin D levels.
If you are getting at least 15 minutes of daily sunlight exposure (without sunscreen) and your blood Vitamin D level is still low, talk to your health care provider or Registered Dietitian Nutritionist to determine the dose of supplemental Vitamin D3 that is appropriate to get you to the optimal range. Many practitioners feel optimal serum Vitamin D levels should be between 50 – 80 nmols/L. For some people, short term supplementation may correct the deficiency while for others, daily supplemental Vitamin D3 may be necessary long term. Also, make sure you are getting adequate magnesium in your diet daily.
Magnesium
Magnesium is necessary for over 300 enzyme systems in the body including helping to convert Vitamin D to its active form so it can turn on calcium absorption. A diet low in magnesium can result in low blood levels of Vitamin D in spite of daily supplementation with Vitamin D. Earlier human diets that included a wide variety of whole foods contained much higher levels of magnesium than today’s Standard American Diet (SAD) which consists of highly processed foods and only about 200 mg of magnesium daily. The RDA for magnesium is 300 mg for adult women and 350 mg for adult men.
A diet low in magnesium can cause low levels of Vitamin D in spite of daily Vitamin D supplementation #saslife Share on XMany foods are good sources of magnesium particularly beans, greens, grains, nuts and seeds (remember the acronym B-G-G-N). Check out THIS LIST of magnesium sources and aim for at least 300 mg of dietary magnesium daily.
If you are supplementing with calcium, make sure your calcium supplement contains magnesium. A calcium:magnesium ratio of 2:1 from foods and supplements combined is thought by some researchers to be adequate.
For more information on the benefits of magnesium and bone heath, check out THIS BLOG by Carolyn Dean, MD, ND.
Vitamin K2
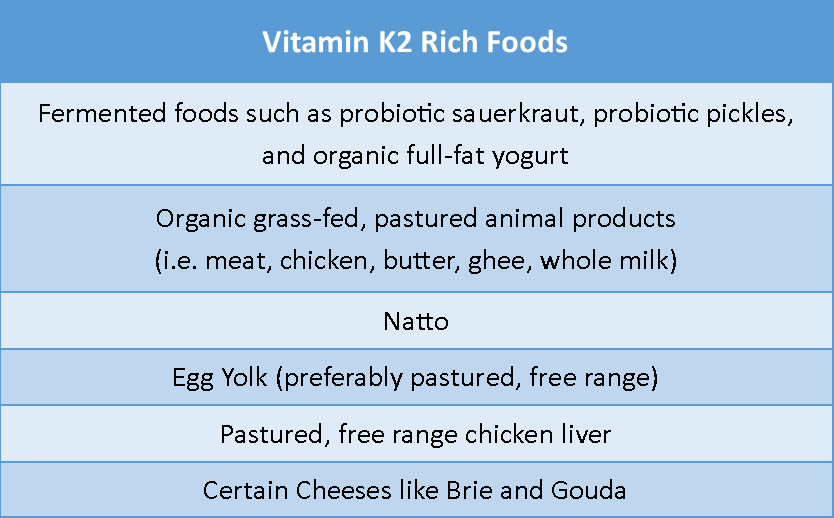
Vitamin K2 is one of the newest kids on the block for bone health. You have likely heard of Vitamin K1 which helps with blood clotting. Vitamin K2 helps deposit calcium where it belongs, in the bones and teeth, and prevents it from depositing in places it does not belong like on artery walls and in soft tissue.
Include foods high in Vitamin K2 in your diet daily.
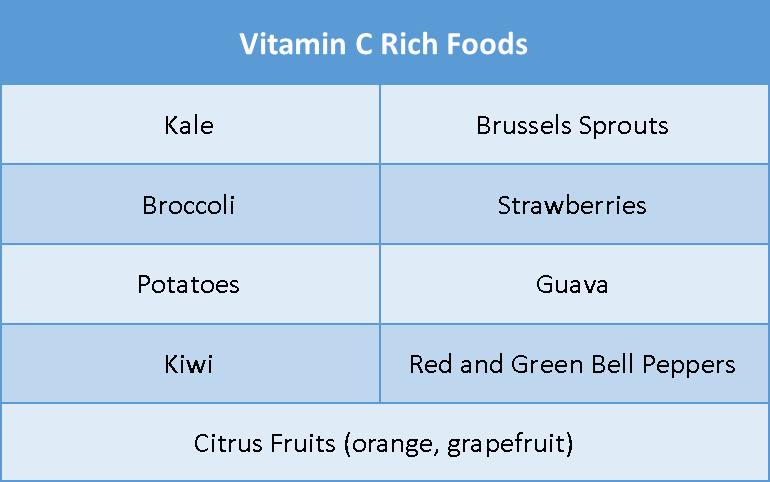
Vitamin C
Vitamin C is essential for collagen formation and bone development. Epidemiological studies have linked low vitamin C intake with bone loss. And, several studies in animals and humans have shown that a diet high in vitamin C prevented or reduced bone loss.
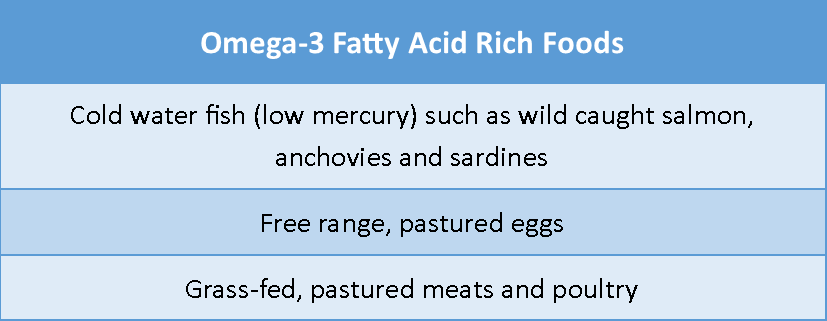
Omega-3 Fatty Acids
Inflammation can lead to bone loss. Omega-3 fatty acids help reduce inflammation. Omega-3s also increase absorption of calcium and decrease excretion of calcium in the urine. Include omega-3 rich fish in your diet 3 times weekly.
You can also consider taking a high quality omega-3 fatty acid supplement that contains 1000 mg of EPA + DHA combined (read the back label for EPA and DHA content of each pill or teaspoonful). Check with your health care provider or Registered Dietitian Nutritionist to see if an omega-3 fatty acid supplement is appropriate for you.
Lifestyle Factors for Bone Health
1. Exercise. Strive for daily movement and include the following exercises that are good for the bones:
- Strength Training – at least 2 times weekly
- Load Bearing Cardio Activity – walking or running – at least 3 times weekly
- Balance Training – daily yoga practice or several times weekly
2. Reduce Stress. Cortisol is one of the body’s stress hormones. Chronic stress can cause chronically high cortisol levels in the body which according to one study could be bad for the bones. Implement the following stress relieving, bone health strategies in your daily life:
- Meditation or HRV Biofeedback training every day – reduces cortisol.
- Exercise, but not too much - excessive intense exercise increases cortisol levels
- Sleep – get 8 hours of restorative sleep each night.
- Include joyful activities in your life every day.
- Spend time outdoors daily.
3. Reduce Inflammation: Chronic inflammation causes bone loss. You can reduce inflammation by:
- eating at least 8 – 10 brightly colored vegetables and 2 fruits daily
- eating the colors of the rainbow daily - ROY G BIV
- reducing stress (see strategies above)
- getting adequate sleep (8 hours per night)
- eliminating or significantly reducing processed carbohydrates and Added Sugar from your eating plan.
Resources:
- Dean, C, “Magnesium is Crucial for Your Bones”, Huffington Post Blog. August 14, 2012.
- Park, Alice, “ Study: US Calcium Guidelines May Be Too High”, Time, May 25, 2011.
- Warensjö, E, et. al., Dietary calcium intake and risk of fracture and osteoporosis: prospective longitudinal cohort study, BMJ 2011;342:d1473
- Harvard Health Publications, “How Much Calcium Do You Really Need?, July 17, 2015.
- Boland, Mark J, et. al., Calcium Intake and Risk of Fracture: Systemic Review, BMJ 2015;351:h4580.
Lemon and Basil Shrimp with Rice
Makes 2 Servings
Adapted From: myrecipes.com
These easy shrimp and rice packets are intended for the oven but they could easily be cooked on the grill or campfire to accommodate your active summer lifestyle.
If you don’t like shrimp, you can substitute wild Alaskan salmon, scallops or any other seafood for the shrimp.
Two 36-inch pieces of heavy duty aluminum foil
Cooking spray
½ cup uncooked wild or sprouted rice (or quinoa)
1 Tbsp extra virgin olive oil
1 cup diced tomato (or 11 grape tomatoes cut into 6ths)
¾ cup sliced green onions (about 3 green onions including the white part)
½ lb fresh asparagus spears, cut into 1 ½ inch pieces
1 clove garlic, minced
½ tsp grated lemon rind
1 Tbsp fresh lemon juice
¼ tsp salt
¼ tsp black pepper
¾ lb large shrimp, peeled and deveined – leave tails attached
1 Tbsp grass fed ghee or butter, melted
¼ tsp seasoned salt or Old Bay Seasoning
¼ cup chopped fresh basil
Directions
Step 1: Make Foil Packets
1.Tear off two 36-inch long pieces of heavy duty foil.
2. Place one piece of foil on top of the other with shiny sides together.
3. Fold one of the long sides over ½ inch and fold over 2 more times to make a sealed edge. Press the edge thoroughly to insure it’s sealed.
4. Now cut the long sheet into equal sized 12x18 inch rectangles.
5. Unfold each rectangle being careful not to pull apart the sealed edge and spray the shiny side of each rectangle with vegetable cooking spray.
6. Place aside for later.
Step 2: Cook Rice and Assemble Ingredients
1. Preheat oven to 450°.
2. Cook the rice according to package directions, omitting salt and oil. (Note: To save time, you can use pre-cooked frozen brown or wild rice).
3. Place the cooked rice in a large mixing bowl.
4. Next, stir in the extra virgin olive oil plus all ingredients through the black pepper.
5. Place half the rice mixture in the middle of each of the large foil sheets.
6. Arrange half the shrimp on each pile of rice mixture.
7. Drizzle the melted butter or ghee over the top of each shrimp.
8. Sprinkled seasoned salt or Old Bay Seasoning on top of each shrimp.
9. Sprinkle each pile with the chopped fresh basil.
10. Bring both long sides of one foil packet up to meet at the top creating a pouch. Place the long edges together and fold over 2 – 3 times. Now, fold each end over 2 – 3 times to seal the pouch. Repeat with the second foil packet.
11. Place both pouches on a baking sheet.
12. Bake at 450° for 25 minutes or until the shrimp are done.
13. Carefully cut open the pouch with a sharp knife being careful of the hot steam.
14. Serve with a tossed salad and seasonal fruit.
Click here for a printer-friendly version of this recipe.
Click here for a printer-friendly version of this blog post.