The emergency department (ED) has always been the front line of patient care – fast, chaotic and often lifesaving. But behind every quick decision made by a clinician, there’s a critical dependency: the lab.
The link between EDs and hospital labs has a rich history, rooted in science, technology and a constant push to improve how we diagnose and treat patients.
A century of progress in lab diagnostics
Going back 100+ years to the early 1900s, Austrian doctor Karl Landsteiner demonstrated in his laboratory that not all blood was the same. He mixed human and animal blood together in his experiments and observed the formation of clots.
When repeating the experiment with human blood from different donors, Landsteiner observed that some donor samples also clumped when mixed and others didn’t. This led to the discovery of the three distinct blood types: A, B and O, for which Landsteiner was given the Nobel Prize in 1930.
It was also in the early 1900s that hospital labs began to really formalize and expand, driven by advances in medical science, such as Landsteiner’s discovery, and the increasing complexity of patient care.
Further, with the commercialization of advanced medical equipment, laboratories started to acquire these specialized tools, such as microscopes, centrifuges and chemical analyzers, allowing for more accurate and varied testing. Blood tests, bacterial cultures and chemical analyses became routine tasks in labs.
Back then, EDs had no flashing monitors, sophisticated triage systems or equipment – only the observing eyes and quick hands of doctors and nurses who relied on their instincts and experience.
But as the knowledge of diseases grew, chemical pathology/clinical biochemistry emerged as a distinct discipline, focusing on the analysis of body fluids and tissues from living patients – until then, most research was done on deceased patients. Laboratory work became more closely integrated with clinical practice, providing critical information for diagnosis and treatment and thereby becoming an important asset to the diagnostic process in EDs.
Fast forward to today: Emergency rooms are still under pressure to move fast; every second still counts. But lab diagnostics, while essential, often slow things down. Patients wait anxiously for lab results, while clinicians balance the urgency of care with the delays inherent in the systems.
What if we could speed all that up without sacrificing accuracy? That’s exactly what Professor Dr. Ivan Brandslund and Hospital Lillebælt in Denmark set out to do – with help from AI, automation and real-time data.
3 pillars to achieve better, safer, faster and cheaper emergency care
The partnership between Professor Dr. Ivan Brandslund and SAS has led to a complete reimagining of diagnostic care in emergency settings. The key? A seamless blend of automation, AI and clinical data. Here’s how it’s changing everything
- Automation – enhancing efficiency and reducing human errors
- Real-time clinical data streaming – enabling faster, data-driven decisions.
- Practical AI – delivering low-latency insights at the point of care.
Automation: Enhancing efficiency and reducing human error
Since the mid-80s, the Lab at Hospital Lillebælt has worked on optimizing and automating the laboratory for the purpose of improving quality and patient outcomes. By 2015, they had a fully digitalized and automated lab with an integrated tube system across the entire hospital with direct transfers of blood samples to the centralized laboratory in 30 seconds.

In 2016, Professor Dr. Ivan Brandslund & Hospital Lillebælt partnered with SAS to develop a groundbreaking solution to disrupt the very foundations of diagnostic care and patient flow in the ED. By integrating advanced technologies like AI and real-time data exchange, the solution redefines how EDs and laboratories work together.
Gone are the days of lengthy waits and fragmented communication. Lab results are now delivered in under 60 minutes and enhanced with AI models that predict the most likely outcome and diagnosis of each individual patient.
How the automation works
A key element of this transformation is the Diagnostic Expert System Enter Real Time (DeSeRT), a hospital-wide initiative. This defines a standardized set of diagnostic tests and data points aimed at delivering early, accurate assessments for emergency patients.
Figure 1 illustrates the fully automated flow of a blood sample in the future emergency department augmented by AI (steps 6-8). The process begins with a patient having their blood drawn, using an analysis panel defined by the DeSeRT protocol (step 1).
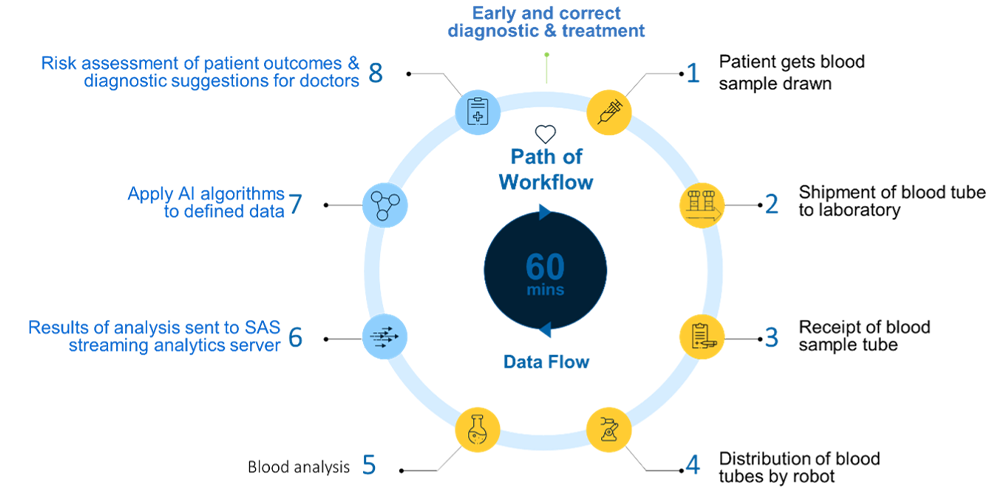
Each sample is uniquely barcoded for identification and sent to the laboratory via the tube mail system. Robots then receive the blood sample and place it in a small "car." The blood sample is then transported via the analysis belt between the various analysis machines (steps 2-5).
When the desired data is available, AI algorithms are applied in real-time to the individual patient's data. The results are compiled into a risk overview, which is then delivered to the doctors in the ED via the hospital’s IT systems (steps 6-8).
This is designed and implemented to take place within approximately 60 minutes, providing doctors with a rapid, AI-augmented second opinion to support their clinical evaluation.
The result is expected to provide a more efficient patient flow and a better patient and clinician experience, ensuring a swift and early diagnosis while enabling the initiation of a treatment plan within the first critical hours in the emergency department.
Real-time clinical data and practical AI
Data selection was absolutely critical from the start to building a reliable, production-ready AI solution for EDs. The project team set a clear requirement: all data used to train the AI models must come from clinical systems capable of providing real-time access and availability, ideally within 60 minutes of admission, facilitating a path from innovation to production.
As shown in Figure 2, the team began with a wide variety of data sources, pulling in a wide range of clinical variables.
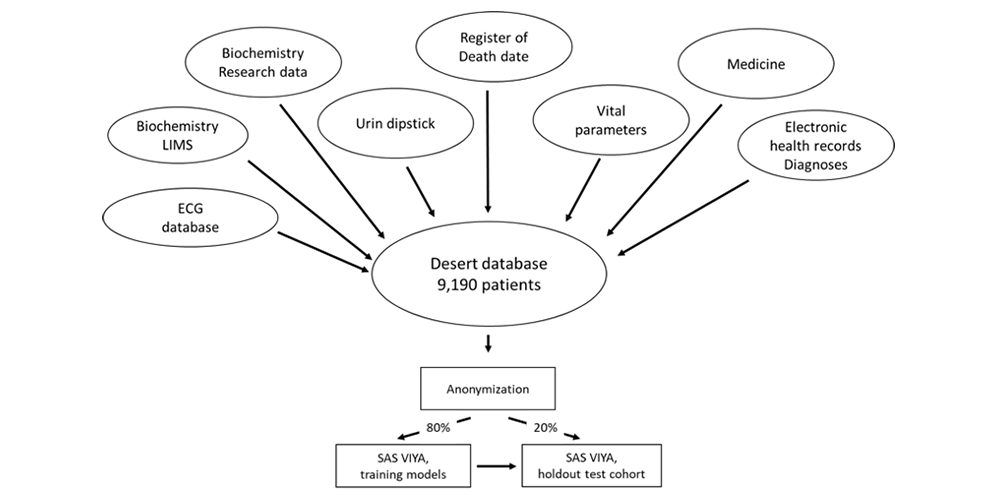
To ensure model accuracy and generalizability, patient data from 9,190 ED admissions were randomly split into two datasets: model training (80%) and a holdout dataset (20%) for validation. This method helped account for seasonal variations in disease patterns and ensured each cohort was representative. The training dataset was used for model development, while the holdout dataset was reserved for evaluating performance reliability. Model training was conducted separately for each target using a variety of approaches, including random forest, gradient boosting, logistic regression and neural networks.
The result: 19 machine learning algorithms were successfully trained and validated, achieving strong performance levels suitable for real-time clinical decision support.
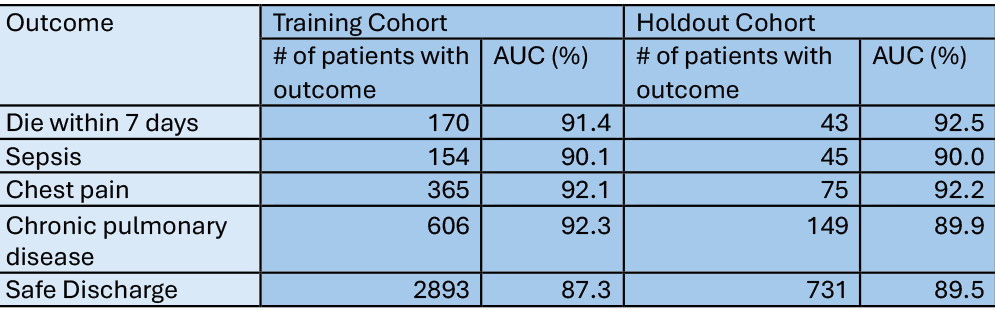
Parts of the promising results from both training and holdout cohorts can be seen in Figure 3 – for the full list of models, refer to the Nature report link at the end of the blog.
The next step was to validate performance and outcomes in a Randomized Controlled Trial (RCT) to assess the anticipated improvements in both patient outcomes and financial goals.
Trustworthy, AI-augmented diagnostics
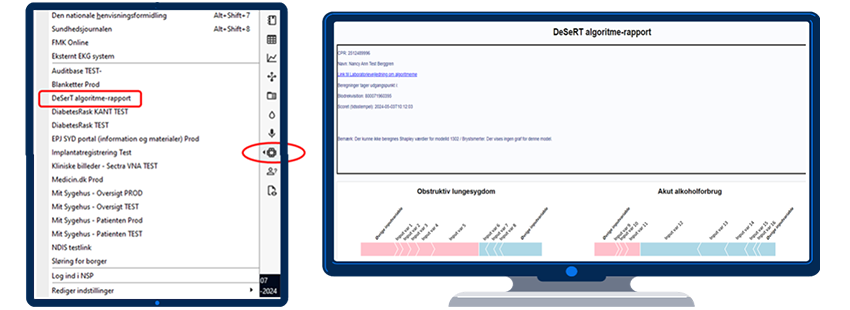
DeSeRT is not an isolated AI solution – it is fully integrated into the local electronic health record (EHR) and laboratory system. Rather than introducing a new, separate application, DeSeRT works within the existing clinical workflow, ensuring that doctors and lab staff can use it without disruption or additional training hurdles.
Built to support – not replace – clinical judgment, DeSeRT provides transparent, real-time insights to help guide diagnostic and treatment decisions. The system’s transparency is a cornerstone of its design: clinicians can easily access and interpret the AI’s reasoning behind each prediction, right from within the EMR.
This is made possible using explainability methods like SHapley Additive exPlanations (SHAP) force plots, which visually show how specific data points contributed to a particular outcome.
It's a new chapter in the history of the link between EDs and laboratories, where the old bottlenecks are a thing of the past and the path to patient recovery is clearer, quicker and more precise than ever before.
Learn about more health care analytics solutions from SAS
Context/disclaimer
Over the past months, Professor Dr. Ivan Brandslund and I have co-authored a chapter in a newly published Danish book exploring the evolution, potential, and ethical challenges of artificial intelligence in health care. Our chapter delves into a project we’ve been developing together since 2016 – an AI-powered diagnostic tool designed to enhance emergency care decision-making. With the project now (hopefully) poised for a Randomized Control Trial, we’re entering an exciting new phase.
This blog offers a sneak peek into the core ideas and outcomes featured in both our book chapter and the accompanying scientific report recently published in Nature. You can find the book here. An English version of the book is expected to be released in the second half of 2025.

